For decades, scientists have been studying the possibility of transplanting animal organs into humans to improve and save people’s lives, especially those in need of organ transplants.
This procedure, known as xenotransplantation, involves transferring living cells, tissues, or organs from animals to humans. Although it has been a topic of debate, many people also want this method to be successful.

Now, would you believe if I told you that recently, scientists have successfully transplanted a genetically edited pig kidney into a living human for the first time?
Amazing, right?
This is an important achievement because it brings us closer to having more available organs for patients who need transplants.
Massachusetts General Hospital (MGH) recently shared news about a successful kidney transplant from a genetically modified pig to a 62-year-old man with end-stage kidney disease (ESKD).
Richard (Rick) Slayman, who suffers from type 2 diabetes and high blood pressure, received the transplant on March 16, 2024, and the surgery lasted around four hours.

Mass General Brigham, known for its advanced transplantation services, was responsible for this groundbreaking achievement.
The pig kidney was provided by eGenesis, a pharmaceutical firm based in Cambridge, and the pig donor was genetically edited using CRISPR-Cas9 technology.
This technology removes certain pig genes that produce sugars with antibodies our immune systems react to.
It also adds certain human genes to improve the kidney’s compatibility with humans, specifically human genes to enhance its compatibility with humans.
Lastly, it deactivates viruses that exist in all pig genomes, called porcine endogenous retroviruses, to reduce the risk of infection in humans.

Slayman also received new monoclonal antibody drugs designed to suppress immune reactions against pig tissue. Two pharmaceutical companies provided these drugs at no cost to Slayman.
In the past, Slayman had already received a human kidney transplant, but unfortunately, it started failing after five years. Because of this, he ended up going back to dialysis treatment due to end-stage kidney failure. He had to make regular hospital visits to manage the complications caused by dialysis.
Good News
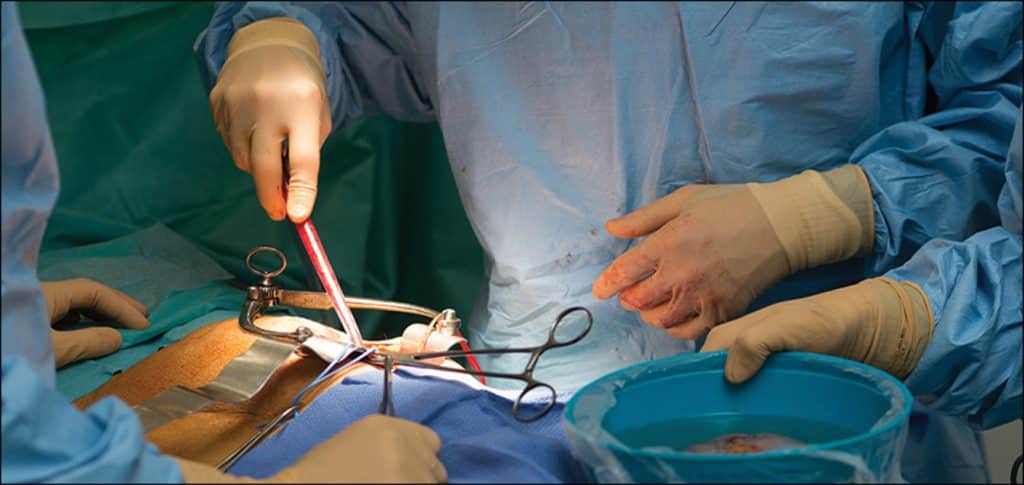
After the surgical team, consisting of Dr. Riella, Dr. Kawai, and Dr. Nahel Elias, finished connecting the kidney, the new organ immediately showed healthy signs, according to Dr. Winfred Williams, Slayman’s nephrologist.

Image credit: Michelle Rose/Massachusetts General Hospital
The ureter was producing urine, and the team’s success was met with applause. Almost a week after the operation, Slayman is recovering well and will soon be discharged.
According to Dr. Madsen, the real hero of this pioneering surgery is Mr. Slayman, whose courage and willingness to embark on a journey into uncharted medical territory made this once unimaginable success possible.
Addressing A Critical Need
Animal organs have been used for transplanting into humans in the past. Recently, two terminally ill patients, David Bennett, Sr. and Lawrence Facuette, received pig hearts from the University of Maryland.
Sadly, both patients passed away. David Bennett died because of heart failure, while Lawrence Facuette showed signs of organ rejection.
Researchers are studying the transplantation of organs or tissues from animals as a solution to the worldwide shortage of donated organs.
The United Network for Organ Sharing reports that over 100,000 people in the U.S. are waiting for an organ transplant, and 17 people die each day waiting for one. Kidneys are the most commonly needed organs.
Chronic kidney disease affects an estimated 36 million people in the U.S., and around 800,000 of them have end-stage kidney disease or kidney failure. This terminal condition requires either a new kidney or painful, prolonged dialysis sessions that can last several hours at a time, several times a week.
Transplanting organs from animals into humans safely requires several steps to minimize the risk of organ rejection by the recipient’s immune system and prevent infection and other complications.
If animal organ transplants for kidneys prove to be safe and effective, they could one day eliminate the need for dialysis for over 500,000 people in the U.S. who depend on it to survive.







